Bynn offers an AI-powered solution for insurance fraud detection that helps carriers process claims faster while keeping fake or tampered documents out of your workflow.
Our cutting-edge document fraud detection system achieves over 99% accuracy in identifying known fraudulent documents, meaning you can confidently approve legitimate claims and stop fraudulent ones in their tracks. By preventing forged evidence from slipping through, Bynn frees up your Special Investigation Unit (SIU) to focus on the fraud cases that truly matter, protecting your bottom line and customer trust.
Coalitions and organizations such as the Coalition Against Insurance Fraud and the National Insurance Crime Bureau (NICB) play a vital role in fighting insurance fraud, with the NICB dedicated to this mission for over 100 years.
Claims Fraud Has Never Been Easier—Or More Dangerous
Modern insurance claims fraud has become alarmingly easy (and dangerous) thanks to readily available digital tools. Anyone with a computer and basic editing software can modify a PDF or image, or even download high-quality fake documents from underground websites. From phony receipts to falsified medical reports, fraudsters have no shortage of resources to create convincing fakes. This surge in accessible forgery techniques means insurers face more fraudulent claims than ever before. To combat this, companies need defenses that are advanced, resilient, and fast. Bynn’s AI-driven platform is built exactly for this challenge – delivering sophisticated fraud detection at machine speed. It uses machine learning models to analyze documents for signs of forgery, detecting subtle alterations invisible to the human eye. With Bynn, insurers get a hardened defense that keeps pace with even the most sophisticated assaults by fraudsters.
The rise of digital technologies has unfortunately made it easier for fraudsters to commit insurance fraud through various sophisticated methods. These include submitting false or misleading information on insurance applications or claims, fabricating documents to support bogus claims, and manipulating images or text in ways that are difficult to detect manually. Insurance agents and fraud divisions within companies are under increasing pressure to identify these deceptive acts quickly to prevent financial losses and protect honest policyholders.

Hard fraud involves deliberate acts such as staging accidents or inventing losses to claim payment, often involving organized groups that can steal millions of dollars. Soft fraud, on the other hand, includes exaggerating legitimate claims or providing misleading information on applications, which collectively contribute to higher premiums for all consumers. The total cost of insurance fraud in the United States alone runs into billions of dollars annually, placing a significant financial burden on the insurance industry and policyholders alike.
Efforts to combat insurance fraud increasingly rely on a combination of advanced AI technologies, data analytics, and collaboration with law enforcement agencies. Organizations like the National Insurance Crime Bureau (NICB) play a vital role in these efforts by collecting intelligence, providing training, and supporting investigations into suspected fraud. By integrating AI-powered fraud detection systems such as Bynn’s with the expertise of fraud investigators and the resources of fraud divisions, insurance companies can more effectively identify and stop fraudulent activities, protect consumers, and reduce the financial impact of fraud on the industry.
.png)

.svg)
Validate Claim Documents in Seconds
Speed is critical when processing insurance claims. Bynn’s solution can verify the authenticity of claim documents in a matter of seconds, allowing you to make decisions faster. There’s no need to manually cross-check with document issuers or delay a claim waiting for verification. As soon as a claimant uploads a document (PDF or image), our system analyzes it in real time using advanced AI. In fact, Bynn provides verification results in under 10 seconds, automatically flagging anything suspicious. This rapid turnaround means valid claims can be approved and paid out quickly. However, increased scrutiny from fraud investigations can sometimes delay the processing of a legitimate claim, but Bynn’s rapid validation helps minimize these delays. While fraudulent submissions are instantly caught and stopped, Bynn’s system also ensures that only claims within the appropriate coverage are approved. Statistical analysis is used to identify fraudulent claims by comparing claim data to expected values, helping to distinguish between legitimate claims and those that are not. The verification can be done seamlessly via API integration or through Bynn’s dashboard, fitting right into your existing claims workflow.
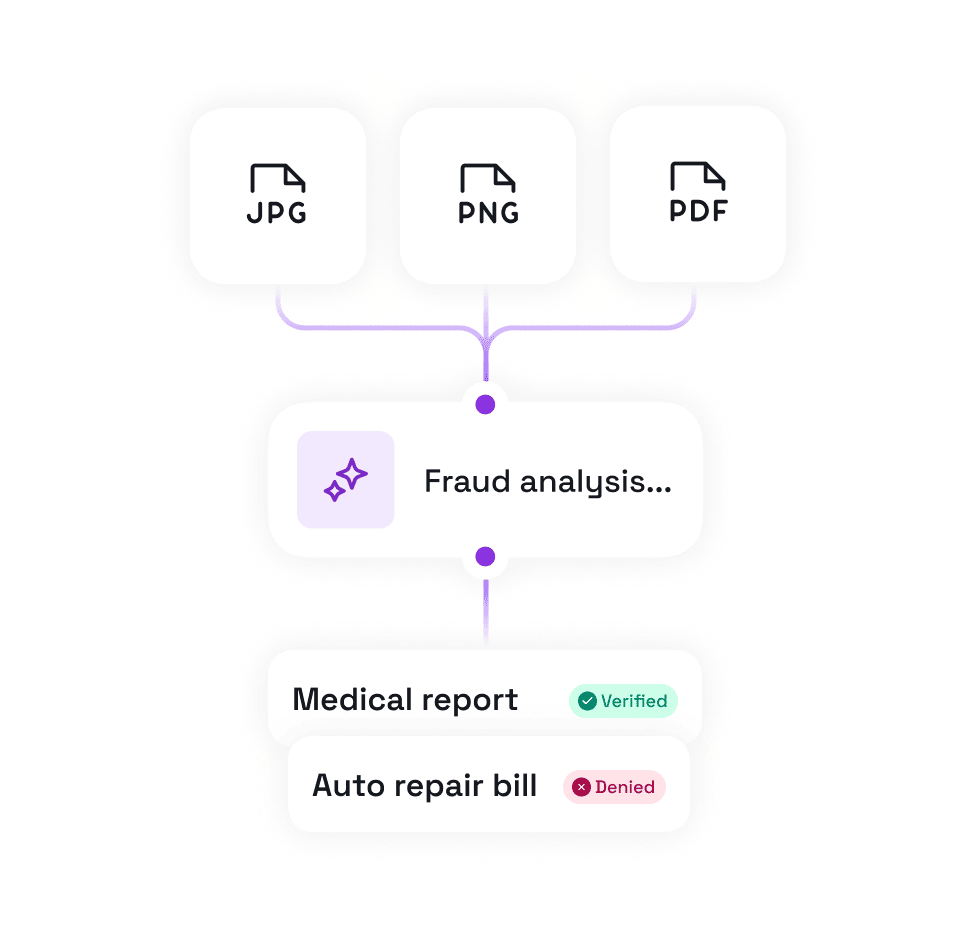
By removing dependence on third-party verifications and using AI to check documents directly, insurers can dramatically speed up claim decisions – improving customer experience and operational efficiency.
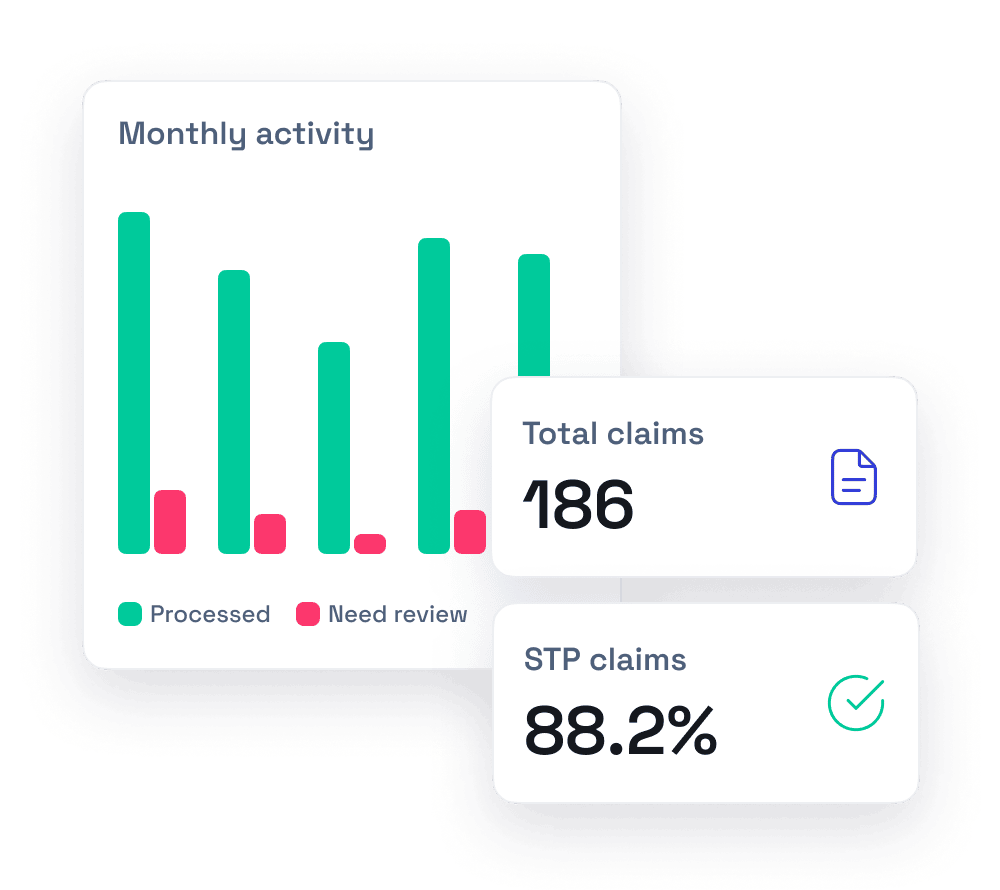
Automate Your Claims Workflow
Bynn’s AI doesn’t just detect fraud; it also helps automate your claim workflows. Insurance fraud can occur at any stage of the insurance transaction, from the initial application to paying claims, through actions such as staging accidents, exaggerating claims, or misreporting information. Our platform automatically fast-tracks good claims and escalates high-risk ones, so your team doesn’t have to review every single file manually. Legitimate claims with authentic documents can be safely straight-through processed (STP) – in fact, over 90% of documents can be cleared without human intervention under Bynn’s system – while the few suspicious cases are immediately flagged for closer inspection. This intelligent routing ensures adjusters and investigators spend time only on the claims that truly need their expertise.
By streamlining operations in this way, you reduce manual workload, minimize human error, and shorten claim processing times. The result is a more efficient claims department that pays out genuine claims faster. Paying claims accurately and promptly is crucial, but fraudulent activities can disrupt this process, leading to delays or denials that impact both insurers and policyholders. For example, if someone submits a doctored repair invoice, Bynn’s detector will catch the altered fields and alert your fraud team, whereas a genuine invoice from a trusted source will pass through to payout without delay. Employers can also be involved in or targeted by workers' compensation fraud, such as by faking injuries to collect benefits. Such automation not only saves time and costs but also creates a consistent, unbiased review process for every claim.
Modernize Your Fraud Defenses with Advanced AI
Staying ahead of emerging fraud tactics requires state-of-the-art AI capabilities, and that’s exactly what Bynn delivers. We’ve poured years of expertise into training our AI on all types of document fraud – from traditional forgeries to the latest digital manipulations. Bynn’s system can spot signs of fraud through hundreds of different indicators, giving you a 360° analysis of each document’s authenticity. It performs cross-field consistency checks (examining fonts, layouts, and data fields for mismatches) to catch even subtle tampering. It also verifies document integrity against known trusted records; for instance, our solution can compare an uploaded invoice to patterns from trusted invoices collected since 2003, providing a baseline to detect anomalies.

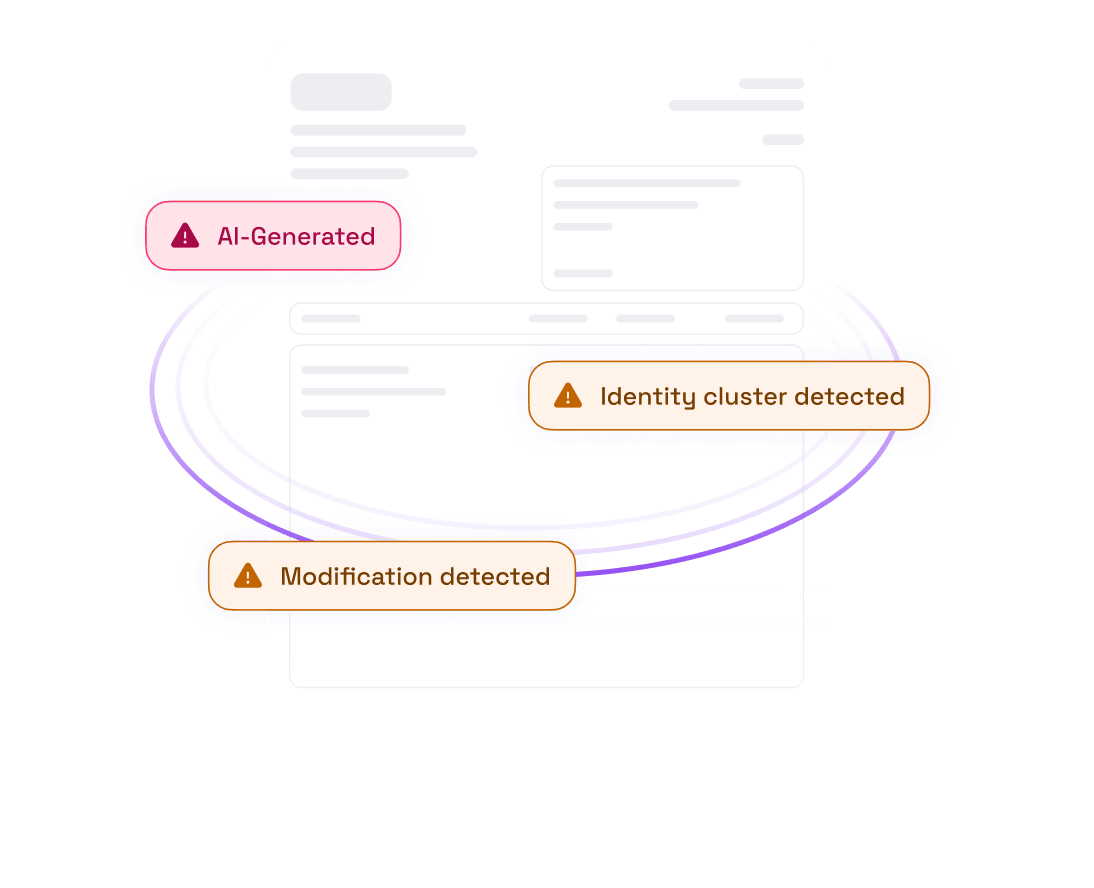
Crucially, Bynn keeps you protected against next-generation fraud schemes as well. Our platform is equipped to identify sophisticated deepfake elements in documents and detect content that has been machine-generated by AI. This means even if a fraudster uses generative AI to create a fake police report or manipulates an image using deepfake techniques, Bynn’s advanced detectors will recognize the telltale signs. We maintain a continuously updated database with over 200,000 known forgery templates – from fake receipt templates circulating on the dark web to forged medical form layouts – which our AI references to spot template-based forgeries instantly. The National Insurance Crime Bureau (NICB), a non-profit organization, also plays a key role by processing questionable or suspected fraud claims and providing training for law enforcement to combat insurance fraud. Moreover, Bynn’s dedicated fraud lab of experts is always researching new fraud patterns and feeding those insights into our models. Organizations like the NICB work closely with their members—including insurance companies, law enforcement, and consumers—to combat insurance fraud and theft, supporting a collaborative approach to industry protection.

.png)
Our advanced AI has been rigorously validated on a dataset of more than 30 million manipulated documents collected over decades, achieving industry-leading detection accuracy. In short, Bynn helps modernize your fraud defenses by combining data-driven machine learning and expert knowledge, giving your insurance company an ever-evolving shield against fraud. With these advanced capabilities, insurers can confidently fight fraud, waste, and abuse in insurance claims, knowing that even the most sophisticated scams will be uncovered. Identifying suspected fraud, especially in high-risk areas like auto insurance where organized schemes and staged collisions are prevalent, is critical to protecting both insurers and their members.
Comprehensive Fraud Prevention for Insurance Companies
Insurance fraud doesn’t only involve fake documents – it can span identity theft, impersonation, and other deceitful tactics. Bynn provides a comprehensive suite of fraud prevention tools that can safeguard every step of your insurance process, from underwriting to claims payout. Life insurance fraud often occurs at the application stage, with applicants misrepresenting their income and personal information to obtain better coverage or lower premiums. Our platform can be tailored to the needs of insurers, combining document forensics with additional verification services to create a multi-layered defense. Health insurance fraud, including Medicare fraud, is a significant issue, costing the U.S. healthcare industry about $51 billion annually and often involving false claims, identity theft, and misrepresentation of eligibility. Beyond document checks, Bynn offers:
- Identity Verification (KYC)
- Proof of Address & Utility Bill Verification
- Phone and Email Verification
- Proxy & Anonymous IP Detection
- Advanced Customer Risk Assessment
End-to-end fraud protection
By integrating these tools alongside document fraud detection, insurance companies get end-to-end fraud protection. Protecting your family from insurance fraud is crucial, as fraud can increase premiums for the average U.S. family by $400 to $700 annually. Whether it’s a fake medical bill, a staged accident claim with synthetic identities, or a policyholder providing false information, Bynn’s platform has the capabilities to detect it. All these services work in harmony, and thanks to flexible APIs and SDKs, integration is seamless. You can easily plug Bynn’s solutions into your existing claims management systems or workflows without disruption.
The end result is a fraud prevention ecosystem that not only catches document forgery but also fortifies every touchpoint of the insurance lifecycle – giving you confidence that both your claims and underwriting processes are secure from fraud. Consumers should verify the legitimacy of insurance companies or agents with their state insurance department before purchasing a policy, and report suspected insurance fraud to the department or special fraud bureaus.

.png)
Conclusion and Future Directions
Insurance fraud remains a persistent threat with a significant financial impact on both insurance companies and consumers. Understanding the difference between hard fraud and soft fraud is crucial for developing effective prevention and detection strategies. The integration of AI and machine learning has provided powerful new tools in the fight against fraudulent activities, but it is essential to recognize and address the limitations of these technologies.
Collaboration among insurance companies, law enforcement agencies, and organizations like the National Insurance Crime Bureau is key to protecting consumers and maintaining the integrity of the insurance industry. As new forms of fraud emerge and criminals adapt their tactics, the industry must remain vigilant and continue to evolve its defenses. By fostering transparency, supporting innovation, and working together, the insurance sector can reduce the costs associated with fraud, ensure that claims are paid fairly, and protect the interests of all policyholders.

.png)
Insurance fraud remains a persistent threat with a significant financial impact on both insurance companies and consumers. Understanding the difference between hard fraud and soft fraud is crucial for developing effective prevention and detection strategies. The integration of AI and machine learning has provided powerful new tools in the fight against fraudulent activities, but it is essential to recognize and address the limitations of these technologies.
Collaboration among insurance companies, law enforcement agencies, and organizations like the National Insurance Crime Bureau is key to protecting consumers and maintaining the integrity of the insurance industry. As new forms of fraud emerge and criminals adapt their tactics, the industry must remain vigilant and continue to evolve its defenses. By fostering transparency, supporting innovation, and working together, the insurance sector can reduce the costs associated with fraud, ensure that claims are paid fairly, and protect the interests of all policyholders.
.png)
